What Low Magnesium Levels Mean for Atrial Fibrillation
Table of Contents

Have you ever wondered why your heart sometimes skips a beat or feels out of rhythm? Your body needs the right balance of minerals to keep your heart healthy. Low magnesium levels can make your heart’s rhythm less stable. Studies show that people with low magnesium have a higher risk of atrial fibrillation. The table below shows how often atrial fibrillation occurs in people with different magnesium levels:
| Magnesium Level (mg/dL) | Rate of Atrial Fibrillation (per 1000 person-years) |
|---|---|
| ≤1.77 | 9.4 |
| ≥1.99 | 6.3 |
Magnesium Levels and Heart Rhythm
Why Magnesium Matters
You might not think about magnesium every day, but your heart depends on it. This mineral helps your heart keep a steady beat. When your magnesium levels drop, your heart’s electrical system can become unstable. This can raise your risk of af, which stands for atrial fibrillation. Many people in hospitals have low magnesium, but doctors do not always check for it. In one study, 42% of patients had low magnesium, but only 7% got tested. If you have low magnesium, you may face a higher chance of heart rhythm problems.
Tip: Ask your doctor to check your magnesium levels if you have heart rhythm concerns.
How Magnesium Affects the Heart
Magnesium works inside your heart cells to keep everything running smoothly. It controls how certain ions, like calcium, potassium, and sodium, move in and out of cells. These ions help your heart send electrical signals. When you have enough magnesium, your heart can respond well and keep a normal rhythm. Here are some ways magnesium supports your heart:
- It helps control potassium channels, which affect how long each heartbeat lasts.
- It slows down signals in the atrioventricular node, which helps prevent abnormal rhythms.
- It stops blood vessels from tightening too much, which helps keep blood pressure steady.
- It keeps potassium from leaving your cells, which is important for a healthy heartbeat.
If your magnesium levels get too low, your heart cells can become unstable. This can lead to changes in energy use and ion movement, making arrhythmias more likely. Low magnesium can also cause your heart cells to become more excitable, which may trigger irregular beats. Inflammation in the heart can also happen when magnesium is low, adding to the risk of rhythm problems.
What Is Atrial Fibrillation?
Understanding Arrhythmias
Your heart uses electrical signals to keep a steady rhythm. Sometimes, these signals get mixed up. When this happens, you may have an arrhythmia. An arrhythmia means your heart beats too fast, too slow, or in an irregular way. Many types of arrhythmias exist, but some are more common than others.
- Atrial fibrillation affects about 4.9% of people in certain studies.
- Other arrhythmias are even more common, with a prevalence of 8.4%.
- As you get older, your risk of atrial fibrillation goes up. For example, 3% of people aged 60-66 have it, but this rises to 7.4% for those aged 81-87.
Atrial fibrillation stands out because it causes the upper chambers of your heart to quiver instead of beating smoothly. This can make your pulse feel fast or uneven. You might notice your heart racing, fluttering, or skipping beats.
Note: In 2017, doctors found about 3 million new cases of atrial fibrillation worldwide. The incidence of atrial fibrillation reached 403 cases per million people that year. This number has grown by 31% since 1997.
Why Atrial Fibrillation Is Serious
You should not ignore atrial fibrillation. This condition can lead to major health problems if left untreated. Here are some of the biggest risks:
- Stroke: Blood clots can form in your heart and travel to your brain, making you up to five times more likely to have a stroke.
- Heart Failure: Your heart may not pump blood well, causing tiredness, trouble breathing, and fluid in your lungs.
- Cognitive Decline and Dementia: Poor blood flow and a higher risk of strokes can hurt your memory and thinking skills.
Atrial fibrillation can change your life. You may feel tired, dizzy, or short of breath. If you notice these symptoms, talk to your doctor. Early treatment can help you avoid serious problems and keep your heart healthy.
Magnesium Levels and Atrial Fibrillation Incidence
Research on Magnesium and AF
You may wonder how magnesium levels connect to atrial fibrillation. Many large studies have looked at this question. Researchers found that low serum magnesium increases the risk of af. For example, the Framingham Heart Study showed a strong association between serum magnesium and atrial fibrillation incidence. People with the lowest serum magnesium had about a 30% higher risk of af than those with higher levels. This means that hypomagnesemia predisposes to af, especially when your levels drop below a certain point.
- Large-scale cohort studies link low serum magnesium to increased risk of af.
- The risk of incident af rises sharply in the lowest quartile of serum magnesium.
- The association between serum magnesium and atrial fibrillation incidence is not always linear. The risk seems to jump when you reach a threshold.
If you have magnesium deficiency, you may face a higher chance of developing atrial fibrillation. This is true even if you do not have other heart problems. After cardiac surgery, patients with atrial fibrillation often show changes in serum magnesium. Some studies suggest that magnesium administration, such as magnesium sulfate, can affect the development of atrial fibrillation after surgery. However, the evidence is mixed. Some research found that higher magnesium levels after surgery linked to more cases of postoperative atrial fibrillation, while other studies suggest that hypomagnesemia can also be a risk factor.
Note: Doctors sometimes use magnesium sulfate as a treatment for acute atrial fibrillation with rapid ventricular response. Some studies show it can help lower the heart rate when used with other treatments. Other research finds no clear benefit, so the role of magnesium in treatment remains uncertain.
Serum vs. Dietary Magnesium
You might think eating more magnesium-rich foods will protect you from atrial fibrillation. The story is more complex. Studies show that serum magnesium levels have a much stronger association with atrial fibrillation incidence than dietary intake. When researchers looked at dietary magnesium, they did not find a significant link to the risk of af. This may be because food surveys do not always measure your true intake. Your body’s magnesium levels depend on more than just what you eat.
- Serum magnesium levels predict the risk of af better than dietary intake.
- Dietary magnesium intake does not show a strong association with atrial fibrillation.
- Food frequency questionnaires can lead to errors in measuring magnesium intake.
If you already have low serum magnesium, eating more magnesium may not always fix the problem. Some people need supplements or medical help to correct a deficiency. Magnesium sulfate, given by IV, may help some patients with atrial fibrillation, but the evidence is not conclusive. You should talk to your doctor before starting any new supplement or treatment.
Tip: If you have symptoms or risk factors for magnesium deficiency, ask your doctor to check your serum magnesium. This test gives a clearer picture of your risk of af than diet alone.
Development of Atrial Fibrillation: Risk Factors
Symptoms of Low Magnesium
You may notice certain signs when your body does not have enough magnesium. These symptoms can warn you about possible problems with your heart rhythm and the development of atrial fibrillation. If you feel muscle twitches or cramps, you should pay attention. You might also experience fatigue or muscle weakness. Some people report numbness or abnormal eye movements. Mental health conditions, such as feeling anxious or depressed, can also appear. In rare cases, convulsions may happen.
Here is a table showing the most common symptoms of magnesium deficiency:
| Symptoms |
|---|
| Muscle twitches |
| Cramps |
| Mental health conditions |
| Fatigue |
| Muscle weakness |
| Abnormal eye movements (nystagmus) |
| Convulsions |
| Numbness |
If you notice these symptoms, you may have a higher risk of af. Magnesium deficiency can make your heart cells unstable. This instability can lead to the development of atrial fibrillation, especially if you already have other risk factors.
Who Is at Risk
You may wonder who faces the greatest risk of incident af and magnesium deficiency. Older adults, especially those over 80, have a higher chance of low serum magnesium and the development of atrial fibrillation. People with lower education levels also show increased vulnerability. Patients with atrial fibrillation often have lower magnesium concentrations. Both continuous and intermittent forms of atrial fibrillation appear more often in these groups.
Lifestyle and medical factors can increase your risk. Here are some important risk factors:
- Age: Your body absorbs less magnesium as you get older.
- Alcohol dependence: Drinking more alcohol can lower your magnesium levels.
- Medical conditions: Type 2 diabetes and stomach or bowel diseases can affect magnesium absorption.
- Dietary choices: Eating a poor diet can lead to deficiency.
- Pregnancy or breastfeeding: Your body needs more magnesium during these times.
- Medications: Diuretics and other drugs can cause magnesium loss.
- Increased intake of vitamin D and phosphorus: These nutrients can raise your magnesium needs.
- Drinking soft drinks with phosphoric acid: This can lower your magnesium levels.
If you have several risk factors, you may see a higher cumulative incidence of af. Hypomagnesemia and magnesium deficiency can make the development of atrial fibrillation more likely. Magnesium administration may help some people, but you should always talk to your doctor about treatment options. If you have rapid ventricular response or other heart symptoms, seek medical advice.
Managing Magnesium Levels

Testing for Deficiency
You may wonder how doctors check your magnesium levels. The most common way is a blood test for serum magnesium. This test is simple and easy to get. However, it does not always show if your body has enough magnesium. Serum magnesium makes up less than 1% of your total magnesium stores. Sometimes, your blood test looks normal even when your body is low. This can make magnesium deficiency hard to spot.
Other tests can give more information. Some doctors use urine tests or check magnesium in red blood cells. These tests can help if you have symptoms but normal serum magnesium. The table below shows different ways to check magnesium status, along with their pros and cons:
| Method | Advantages | Limitations |
|---|---|---|
| Total serum/plasma magnesium | Simple and widely used | Not sensitive for body stores; may miss CLMD |
| Plasma ionized magnesium | Measures active form | May still miss deficiency |
| Urinary magnesium excretion | Shows intake | One test may not reflect stores |
| Magnesium load test | Valid assessment | Invasive, time-consuming |
| Erythrocyte magnesium | Assesses body stores | Laborious, not routine |
| Muscle magnesium | Direct assessment | Very invasive, needs skill |
| Buccal cell magnesium | Direct assessment | Needs skill, expensive equipment |
Note: Serum magnesium can look normal even if your body is low. Many factors can affect the results.
Boosting Magnesium Intake
You can support your heart by eating foods rich in magnesium. Some of the best sources include rice bran, tofu, spinach, pumpkin seeds, and almonds. Try to add these foods to your meals each week. Here are some top choices:
- Rice bran (1 cup): 922 mg
- Spinach (1 cup cooked): 157 mg
- Pumpkin seeds (1 oz): 156 mg
- Tofu (1 cup): 146 mg
- Lima beans (1 cup cooked): 126 mg
- Almonds (1 oz): 77 mg
Most adults need 400–420 mg of magnesium each day if you are male, or 310–320 mg if you are female. Pregnant women need a bit more. The chart below shows the recommended daily intake for adults:
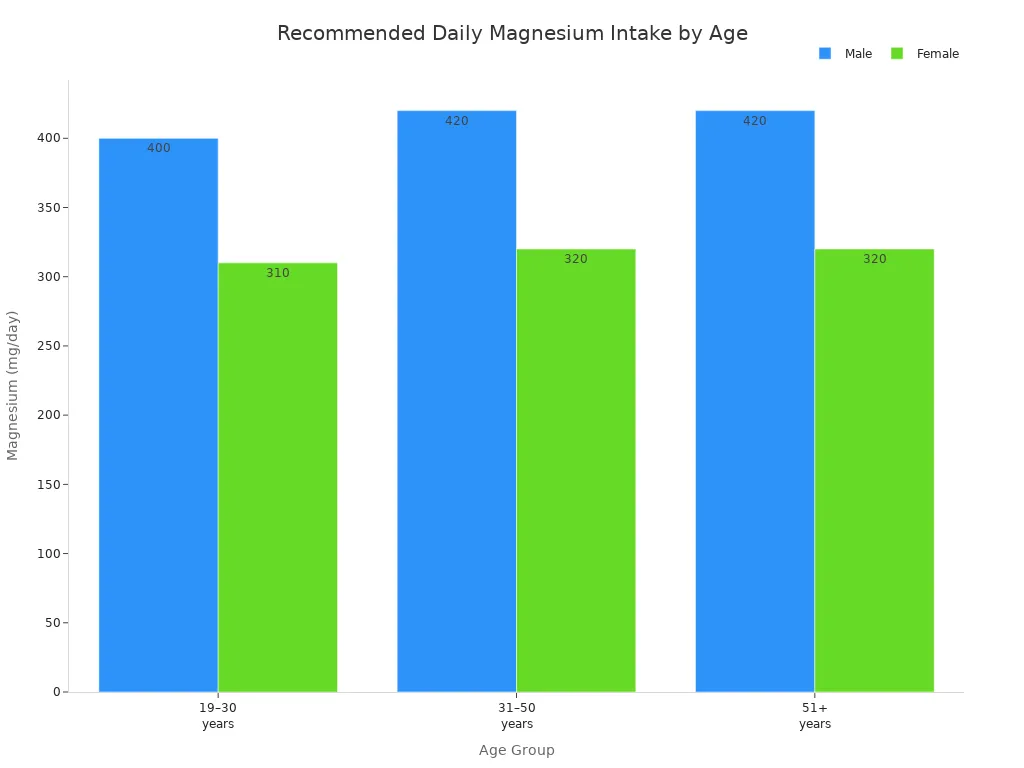
If you have hypomagnesemia or ongoing deficiency, food may not be enough. Your doctor may suggest magnesium supplements or magnesium sulfate. Magnesium administration, such as magnesium sulfate, can help in some cases, especially if you have a low association between serum magnesium and heart rhythm. Always talk to your doctor before starting supplements.
Tip: Eating a variety of magnesium-rich foods helps keep your magnesium levels steady and supports a healthy heart. If you have symptoms or a known association between serum magnesium and atrial fibrillation, regular testing and medical advice are important.
Preventing Atrial Fibrillation
Healthy Habits
You can lower your chance of atrial fibrillation by making healthy choices every day. Doctors say that lifestyle changes play a big role in keeping your heart rhythm steady. You should focus on the risk factors you can control. Here are some steps you can take:
- Lose weight if you are overweight. Even a small amount of weight loss can help your heart.
- Move your body more. Try to get at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise each week.
- Limit alcohol. Drink no more than one drink per day.
- Stop smoking. Quitting helps your heart and lungs.
- Keep your blood pressure and diabetes under control. These conditions make atrial fibrillation more likely.
Managing sleep apnea is also important. If you snore or feel tired during the day, talk to your doctor about testing for sleep apnea. Treating this condition can cut your risk in half.
You should eat foods high in magnesium, such as leafy greens and nuts. These foods support your heart and help keep your rhythm normal.
When to See a Doctor
You need to know when to get medical help for atrial fibrillation or low magnesium. Some warning signs mean you should see a doctor right away. Look at the table below for symptoms that need attention:
| Warning Sign | What It Means |
|---|---|
| Numbness and Tingling | You feel pins and needles in your hands or feet. |
| Tightness of Breath and Asthma | You have trouble breathing or your asthma gets worse. |
| Abnormal Heart Rhythm | Your heart feels like it skips, flutters, or beats too fast. |
| High Blood Pressure | Your blood pressure is higher than normal. |
| Nausea and Vomiting | You feel sick to your stomach or throw up, especially with other signs. |
You should also see your healthcare provider if you notice new symptoms or if your treatment does not work. Regular check-ups help you stay on track. If you think you have atrial fibrillation, check your pulse and call your doctor. Watch for signs of stroke, such as sudden weakness, trouble speaking, or face drooping. Use the FAST guideline to remember these signs.
Tip: Early action can prevent serious problems. Never ignore changes in your heart rhythm or health.
Keeping your magnesium levels in a healthy range helps your heart beat steadily and may lower your risk of atrial fibrillation. Studies show that good magnesium intake supports heart rhythm by improving blood vessel health. You can choose foods like leafy greens, nuts, and whole grains, and talk to your doctor about regular blood tests.
| Strategy Type | Recommendations |
|---|---|
| Dietary Sources | Leafy greens, nuts, seeds, whole grains, mineral water |
| Lifestyle Changes | Reduce stress, limit alcohol, get enough sleep |
| Supplementation | Ask your doctor about safe magnesium supplements if you need them |
Stay proactive about your heart health. Small steps today can make a big difference for your future.
FAQ
Can magnesium in drinking water help your heart?
You get magnesium in drinking water from natural sources. This mineral helps your heart keep a steady rate. Many studies show that magnesium in drinking water supports healthy heart rhythm. You should check the magnesium concentration in drinking water in your area to see if you get enough.
How does magnesium concentration in drinking water affect atrial fibrillation?
Magnesium concentration in drinking water can change your risk for atrial fibrillation. If you drink water with a higher magnesium concentration in drinking water, your heart rate may stay more regular. Low magnesium in drinking water may raise your rate of heart rhythm problems.
What is the best rate of magnesium in drinking water for heart health?
Doctors recommend a certain rate of magnesium in drinking water for heart health. You should look for water with a magnesium concentration in drinking water that meets these guidelines. A good rate helps your heart beat normally and lowers your risk of atrial fibrillation.
Can you get enough magnesium from drinking water alone?
You may not get enough magnesium in drinking water alone. The rate of magnesium concentration in drinking water varies by location. You should eat foods high in magnesium and check your water’s magnesium concentration in drinking water to make sure you meet your daily needs.
Does the rate of magnesium in drinking water change by location?
The rate of magnesium in drinking water changes based on where you live. Some places have a higher magnesium concentration in drinking water. You should ask your local water provider about the rate of magnesium in drinking water in your area to know if you need more from food or supplements.

Poseidon
Master of Nutritional Epidemiology, University of Copenhagen, Herbal Functional Nutrition Researcher
Focus: The scientific application of natural active ingredients such as Tongo Ali, Horny Goat Weed, and Maca to sexual health and metabolic regulation.
Core Focus:
Men: Use a combination of Tongo Ali (an energizing factor) + Maca (an energy reserve) to improve low energy and fluctuating libido.
Women: Use a combination of Horny Goat Weed (a gentle regulator) + Maca (a nutritional synergist) to alleviate low libido and hormonal imbalances.
Stressed/Middle-Aged Adults: This triple-ingredient synergy supports metabolism, physical strength, and intimacy.
Product Concept:
Based on traditional applications and modern research (e.g., Tongo Ali promotes testosterone-enhancing enzyme activity, and icariin provides gentle regulation), we preserve core active ingredients and eschew conceptual packaging—using natural ingredients to address specific needs.
Simply put: I'm a nutritionist who understands "herbal actives." I use scientifically proven ingredients like Tongo Ali, Epimedium, and Maca to help you make "sexual health" and "nutritional support" a daily routine.

 Maca Gold Capsules 90 Count: Dual-Action Defense (Anti-Fatigue + Antioxidant) × Immune Shield | Cellular-Level Endurance Engine
Maca Gold Capsules 90 Count: Dual-Action Defense (Anti-Fatigue + Antioxidant) × Immune Shield | Cellular-Level Endurance Engine