Understanding Hypoallergenic Formula
Table of Contents
A hypoallergenic formula contains broken-down cow’s milk protein. This design helps prevent allergic reactions in a sensitive baby. This formula is for a baby with a cow’s milk protein allergy or sensitivity. This allergy affects up to 3% of infants, making it a common concern. Choosing the right formula can feel overwhelming. A hypoallergenic baby formula offers a solution.
Signs Your Baby Needs a Hypoallergenic Formula

Parents often wonder if their baby’s discomfort is normal or a sign of a problem. A cow’s milk protein allergy can cause a wide range of symptoms. These allergic reactions can appear in the digestive system, on the skin, or even in a baby’s behavior. Recognizing these signs is the first step toward finding a solution and bringing your baby relief.
Digestive Issues
Problems with digestion are the most common indicator of a milk protein allergy. The baby’s immune system may react to the cow’s milk protein in their formula. This response can cause inflammation in the gastrointestinal tract, leading to noticeable symptoms.
Persistent diarrhea is a primary sign. This is not just a loose stool but frequent, watery bowel movements. Sometimes, parents may also see mucus or blood in the diaper. These allergic reactions happen because the allergy increases intestinal permeability, leading to fluid shifts and irritation. Two conditions related to food allergies, FPIES (Food Protein-Induced Enterocolitis Syndrome) and FPIAP (Food Protein-Induced Allergic Proctocolitis), are often responsible for these severe digestion issues.
Other signs of sensitive digestion include:
- Frequent vomiting or spitting up (acid reflux)
- Apparent abdominal pain or gas
- Constipation, with hard, difficult-to-pass stools
- Blood or mucus in the stool
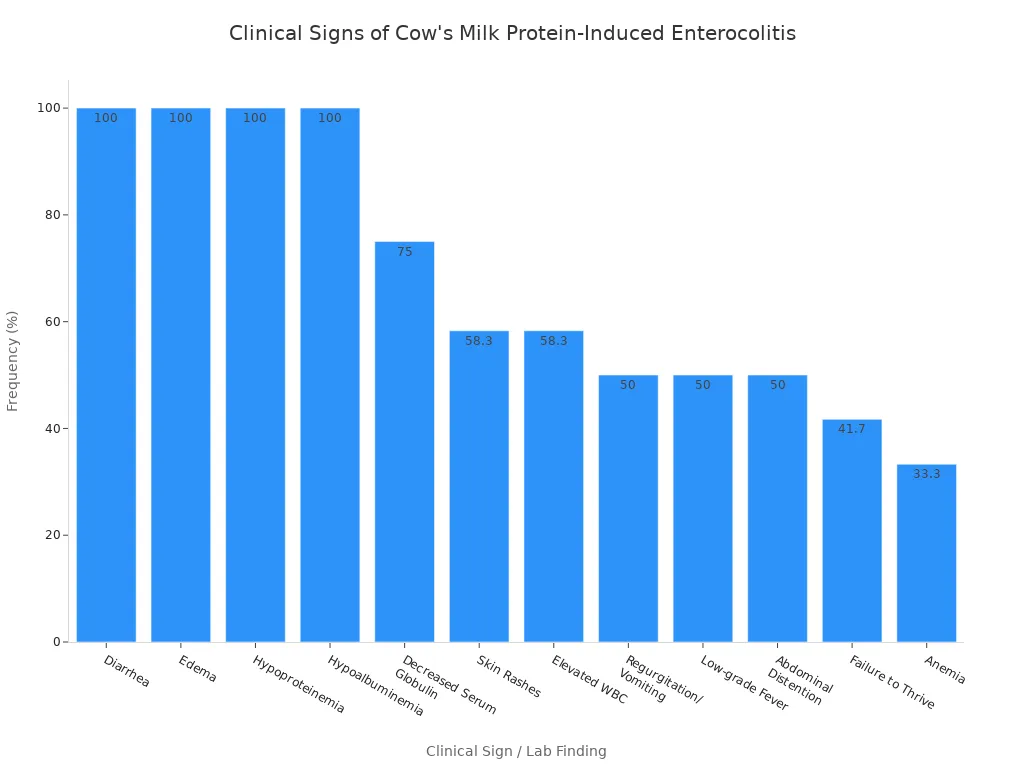
Clinical Signs of Cow’s Milk Protein Allergy A baby with a severe allergy may show multiple symptoms. Research shows the frequency of different clinical signs, highlighting how common digestive issues and other reactions are.
Skin Reactions
A baby’s skin is very delicate. A food allergy can often manifest as a visible skin reaction. These allergic reactions can appear quickly after a feeding or develop over time. The type of rash can help a doctor understand the allergy.
| Reaction Type | Visual Characteristics |
|---|---|
| Rapid Reaction | Raised, itchy red bumps (hives); flushed skin; swelling, often on the face. |
| Delayed Reaction | Patches of dry, scaly, and itchy skin (eczema); rashes that come and go. |
If a baby develops hives or eczema that does not improve with standard care, the formula could be the cause.
Respiratory Symptoms
Respiratory issues are another possible sign of a milk protein allergy. These symptoms can sometimes be mistaken for a common cold because they are so similar. Up to 30% of infants with a cow’s milk protein allergy may experience them. A baby might have a persistent runny nose or sneeze often, sometimes starting within 30 minutes of drinking their formula. More serious symptoms include wheezing or difficulty breathing. Any breathing trouble requires immediate medical attention.
Behavioral Changes
Changes in a baby’s mood and growth can also signal an underlying issue with their formula. A baby who is uncomfortable will often communicate it through their behavior.
One major sign is extreme fussiness or inconsolable crying, often called colic. While the link between colic and food allergies is still debated, some studies show that infants with severe crying experienced relief after switching to a hypoallergenic formula. The constant discomfort from poor digestion can make a baby irritable, especially after feedings.
Another critical indicator is poor weight gain, also known as “failure to thrive.” A cow’s milk protein allergy can contribute to this in several ways. The baby may have a decreased appetite due to discomfort. The inflammation in their gut can also prevent proper absorption of nutrients from their formula. In fact, one study found that 77% of infants with failure to thrive had a disease related to cow’s milk protein allergy. Switching to a hypoallergenic diet helped the majority of these infants achieve healthy catch-up growth.
Types of Hypoallergenic Formulas

Navigating the different types of hypoallergenic formulas can seem complex. Each type offers a different level of protein breakdown. The right choice depends on the baby’s specific needs and the severity of their symptoms. Understanding the three main types of hypoallergenic formulas helps parents and pediatricians make an informed decision.
Partially Hydrolyzed
Partially hydrolyzed formulas contain milk proteins broken into medium-sized pieces, or peptides. These peptides typically have a molecular weight between 3 and 10 kDa. This process makes the formula easier for some infants to digest. The protein structure in a partially hydrolyzed formula may even be closer to that of human milk.
Important Note: The American Academy of Pediatrics does not recommend partially hydrolyzed formulas for a baby with a confirmed cow’s milk allergy. The protein fragments may still be large enough to cause an allergic reaction. This type of formula is not considered truly hypoallergenic for treatment purposes.
Extensively Hydrolyzed
Extensively hydrolyzed formulas are the standard recommendation for infants with a confirmed cow’s milk protein allergy. In this type of hypoallergenic formula, the proteins are broken down into very small peptides. These peptides are generally smaller than 3 kDa, which significantly reduces their potential allergenicity.
This type of formula is highly effective. Studies show that over 90% of infants with a milk allergy see their symptoms improve after switching to an extensively hydrolyzed formula.
- One study reported a 93% improvement in gastrointestinal symptoms.
- Another found that 87.5% of babies experienced relief from skin-related symptoms.
Many popular hypoallergenic baby formulas fall into this category. Brands like Pepticate, which has been used in Europe for decades, and HiPP HA are examples of an extensively hydrolyzed formula designed for medical supervision.
Amino Acid-Based Hypoallergenic Baby Formula
An amino acid-based formula represents the most broken-down option available. This formula does not contain any protein chains or peptides. Instead, it is made from individual amino acids, the basic building blocks of protein. This composition makes an allergic reaction virtually impossible, as there are no protein structures for the immune system to target.
These formulas are often reserved for infants with the most severe conditions. A pediatrician may prescribe an amino acid-based formula for a baby who did not improve on an extensively hydrolyzed formula or for specific medical issues.
Conditions that may require amino acid-based formulas include:
- Severe eosinophilic esophagitis (EoE) or enteropathy
- Complex gastrointestinal conditions
- Protein-losing enteropathy
- Transitioning from intravenous (parenteral) nutrition
The core components of an amino acid-based hypoallergenic baby formula differ significantly from other types, ensuring the lowest possible allergenicity.
| Component | Amino Acid-Based Formula (AAF) | Extensively Hydrolyzed Formula (EHF) |
|---|---|---|
| Protein Source | Free amino acids | Small protein peptides |
| Lactose | Contains no lactose | May contain lactose |
| Allergenicity | Virtually zero | Very low |
Choosing the right formula is a critical step in managing a baby’s health and comfort.
Benefits of Hypoallergenic Formulas
The benefits of hypoallergenic formulas extend beyond basic nutrition. They are a medical tool designed to provide relief and support healthy development. For a baby with a cow’s milk protein allergy, the right formula can be transformative. The main advantages are rapid symptom relief and potential allergy prevention for high-risk infants. These benefits of hypoallergenic formulas offer parents a reliable path toward a happier, more comfortable baby.
Symptom Relief
The most immediate benefit of a hypoallergenic formula is the relief from uncomfortable symptoms caused by allergic reactions. This provides crucial support for sensitive stomachs and helps calm a baby’s system. A switch to the right formula often leads to improved digestion and a noticeable reduction in distress. Many parents see a significant change in their baby’s well-being. The formula helps resolve issues like persistent acid reflux, skin rashes like eczema, and digestive upset.
The timeframe for improvement varies depending on the symptom. A baby may experience relief from some allergic reactions faster than others.
| Symptom Type | Reaction Type | Timeframe for Improvement |
|---|---|---|
| Skin Rashes (Hives) | Immediate | 3-5 days |
| Eczema / Atopic Dermatitis | Delayed | 3-6 weeks for noticeable improvement |
| Digestive Symptoms | Delayed | Up to 4 weeks for full resolution |
| Colic / Fussiness | Delayed | Up to 5 weeks |
This improvement in digestion and overall comfort allows a baby to feed peacefully and absorb nutrients properly.
Allergy Prevention in High-Risk Infants
Certain hypoallergenic formulas may also help prevent food allergies from developing in the first place. This preventative approach is one of the key benefits of hypoallergenic formulas, especially for infants with a high risk of developing an allergy. A high-risk baby typically has a close family member with an allergic condition.
Who is a “High-Risk” Infant?
- The Canadian Paediatric Society defines a high-risk infant as one with a parent or sibling who has asthma, eczema, or food allergies.
- The National Institutes for Allergy and Infectious Diseases (NIAID) considers a baby with severe eczema or an egg allergy to be at high risk for other allergic reactions.
The German Infant Nutritional Intervention (GINI) study provides key evidence for this benefit. The long-term study found that using a specific hydrolyzed formula for high-risk infants reduced the incidence of atopic eczema. This research shows that a hypoallergenic approach can offer protective effects against future allergic reactions.
Choosing and Switching Formulas
Finding the right hypoallergenic formula is a journey best taken with a medical professional. The process involves a proper diagnosis, understanding what to expect, and carefully managing the transition for your baby.
Always Consult a Pediatrician
Parents should always consult a pediatrician before switching to a specialized formula. A doctor can confirm if an allergy is the true cause of a baby’s symptoms. Switching without a diagnosis is not recommended. Studies show that giving partially hydrolyzed formulas to infants without a justified family history of allergies does not prevent them.
A pediatrician uses specific tests to make an accurate diagnosis.
- Skin-Prick Test (SPT): This is an important first step to evaluate a potential food allergy.
- Oral Food Challenge: This test provides a definitive diagnosis by having the baby consume the formula under medical supervision.
What to Expect
Switching to a hypoallergenic baby formula brings several changes. The breakdown of proteins creates bitter peptides, giving the formula a distinct smell and taste that a baby may initially reject. The cost is also a significant factor. Hypoallergenic options are more expensive than standard formula.
| Formula Type | Average Cost Per Ounce |
|---|---|
| Standard Cow’s Milk | ~$0.17 |
| Hypoallergenic | ~$0.30+ |
Parents will also notice changes in their baby’s diapers. Stools often become a different color and consistency. It is normal for a baby on a hypoallergenic formula to have dark green, pasty stools. This happens because the highly broken-down formula is digested differently.
Making the Transition
A gradual transition can help a baby accept the new formula. Parents can start by mixing a small amount of the new formula with the old one. Over several days, they can slowly increase the amount of the new formula until the baby is taking it exclusively. It may take up to three weeks for a baby to fully adjust and for symptoms to improve. Patience is key during this adjustment period.
Hypoallergenic formulas are a medical nutrition solution. They help a baby with a confirmed cow’s milk protein allergy or high allergy risk. Different types of hypoallergenic formula exist to manage varying levels of sensitivity. These options offer significant benefits for the right baby. Choosing the correct formula is a critical decision for a baby’s health.
Important Final Step: A partnership with a pediatrician is the most important step. A doctor ensures the baby receives the best care and the right formula for their specific needs.
FAQ
How long does it take for a baby to improve on a hypoallergenic formula?
Most infants show improvement within two to four weeks. Some allergic reactions, like skin hives, may resolve faster. Full improvement in digestion can take longer. A baby needs time to adjust to the new formula. Patience is important during this transition period.
Can I give my baby a hypoallergenic formula to prevent allergies?
Parents should only use a hypoallergenic formula for prevention in high-risk infants. A doctor can identify if a baby is high-risk. Using this formula without medical advice may not prevent allergic reactions and is not recommended for all infants.
Why does hypoallergenic formula have a different smell and taste?
The process of breaking down cow’s milk protein creates bitter-tasting components. This gives the hypoallergenic baby formula a distinct smell and taste. Many babies need a gradual transition to get used to the new flavor of their hypoallergenic formula.
Are there side effects to using a hypoallergenic formula?
The main changes are in a baby’s digestion. Stools often become dark green and pasty. This is a normal response to the formula. Severe allergic reactions are very rare with a truly hypoallergenic option, as it is designed to prevent them.

Poseidon
Master of Nutritional Epidemiology, University of Copenhagen, Herbal Functional Nutrition Researcher
Focus: The scientific application of natural active ingredients such as Tongo Ali, Horny Goat Weed, and Maca to sexual health and metabolic regulation.
Core Focus:
Men: Use a combination of Tongo Ali (an energizing factor) + Maca (an energy reserve) to improve low energy and fluctuating libido.
Women: Use a combination of Horny Goat Weed (a gentle regulator) + Maca (a nutritional synergist) to alleviate low libido and hormonal imbalances.
Stressed/Middle-Aged Adults: This triple-ingredient synergy supports metabolism, physical strength, and intimacy.
Product Concept:
Based on traditional applications and modern research (e.g., Tongo Ali promotes testosterone-enhancing enzyme activity, and icariin provides gentle regulation), we preserve core active ingredients and eschew conceptual packaging—using natural ingredients to address specific needs.
Simply put: I'm a nutritionist who understands "herbal actives." I use scientifically proven ingredients like Tongo Ali, Epimedium, and Maca to help you make "sexual health" and "nutritional support" a daily routine.
